Understanding DBT Diary Cards
DBT Diary Cards are crucial tools within Dialectical Behavior Therapy (DBT)‚ aiding individuals in tracking emotions‚ behaviors‚ and skill usage daily for enhanced self-awareness.
Free DBT Diary Card PDFs are readily available online‚ offering accessible resources for implementing skills training and monitoring progress in therapy sessions.
Marsha M. Linehan’s work provides comprehensive DBT skills training manuals and handouts‚ including diary cards‚ to facilitate effective emotional regulation and coping strategies.
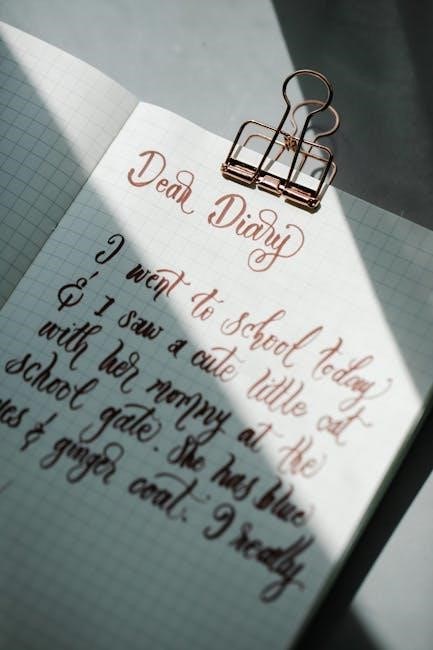
What is a DBT Diary Card?
A DBT Diary Card is a daily record used in Dialectical Behavior Therapy (DBT) to meticulously track specific behaviors and emotional experiences. These cards‚ often available as a DBT Diary Card PDF for convenient download‚ aren’t simply journals; they are structured tools.
They document challenging emotions‚ urges to engage in problematic behaviors‚ and – crucially – the skills the individual attempted to utilize. Resources like those from Behavioral Tech and handouts from Marsha M. Linehan’s DBT Skills Training Manual provide templates.
Completing a diary card fosters self-observation and provides valuable data for therapy sessions‚ aiding in identifying patterns and refining coping strategies.
The Purpose of Tracking with a Diary Card
The primary purpose of utilizing a DBT Diary Card‚ often accessed as a free DBT Diary Card PDF‚ is to increase self-awareness and facilitate behavioral change. Consistent tracking reveals patterns between triggers‚ emotions‚ and maladaptive behaviors.
This detailed record isn’t about judgment‚ but about objective observation. It allows individuals and their therapists to collaboratively identify areas needing focused skill application.
Resources from Linehan’s DBT Skills Training emphasize using the card to monitor skill usage and assess effectiveness‚ ultimately promoting progress towards therapeutic goals and improved emotional regulation.
Components of a Standard DBT Diary Card
DBT Diary Cards typically include sections for tracking emotions‚ behaviors‚ triggers‚ and skills used‚ often available as a downloadable DBT Diary Card PDF.
These cards‚ derived from DBT Skills Training‚ promote detailed self-monitoring for effective therapy.
Tracking Emotions
Tracking emotions on a DBT Diary Card involves noting the specific feelings experienced throughout the day‚ often using a scale to rate their intensity.
A free DBT Diary Card PDF will usually include a dedicated section for listing emotions‚ such as sadness‚ anger‚ fear‚ or joy‚ alongside their corresponding levels.
This detailed recording‚ stemming from DBT Skills Training‚ helps individuals identify emotional patterns and triggers‚ crucial for applying skills like emotional regulation.
Linehan’s manuals emphasize mindful attention to emotions‚ and the diary card facilitates this practice‚ promoting self-awareness and informed coping strategies.
Consistent emotion tracking aids therapists in understanding a client’s emotional landscape.
Monitoring Behaviors
Monitoring behaviors on a DBT Diary Card is essential for identifying problematic patterns and the urge to engage in unhelpful coping mechanisms.
A downloadable DBT Diary Card PDF typically features a section to record specific actions‚ like self-harm‚ substance use‚ or impulsive spending.
This tracking‚ rooted in DBT Skills Training‚ isn’t about judgment‚ but about recognizing behaviors linked to emotional distress and skill deficits.
The goal is to connect behaviors to preceding emotions and triggers‚ enabling the application of distress tolerance and emotional regulation skills.
Behavioral monitoring supports progress tracking within DBT therapy.
Identifying Triggers
Identifying triggers is a core component of utilizing a DBT Diary Card‚ and many free DBT Diary Card PDF resources include dedicated sections for this purpose.
Triggers are events‚ people‚ places‚ or even internal thoughts that precede intense emotional reactions or problematic behaviors.
Recording these on the card‚ alongside associated emotions‚ helps individuals recognize patterns and anticipate challenging situations.
This awareness‚ stemming from DBT Skills Training‚ is crucial for proactively employing coping strategies.
A personalized trigger list‚ added to a standard PDF‚ enhances the card’s effectiveness.
Recording Skills Used
A vital section of any DBT Diary Card PDF is dedicated to Recording Skills Used‚ directly linking practice to real-life application.
This involves noting which DBT skills – mindfulness‚ interpersonal effectiveness‚ emotional regulation‚ or distress tolerance – were attempted in response to difficult situations.
Documenting skill usage‚ even if unsuccessful‚ provides valuable data for therapy.
It helps identify which skills are most effective for specific triggers and emotional states‚ fostering skill development.
DBT Skills Training emphasizes consistent practice‚ and the diary card facilitates this process.

Accessing Free DBT Diary Card PDFs
Numerous DBT Diary Card PDFs are freely available online through websites offering DBT resources‚ including handouts and worksheets for skills training.
Behavioral Tech and other providers offer downloadable PDFs to support individuals in tracking emotions and behaviors.
Online Resources for Downloadable PDFs
DBT resources are widely accessible online‚ offering numerous free Diary Card PDFs for immediate download. Websites dedicated to mental health and DBT skills training frequently provide these valuable tools.
Searching for “DBT Diary Card PDF” yields results from various sources‚ including therapist-created resources and organizations specializing in DBT. These downloadable cards typically include sections for tracking emotions‚ behaviors‚ triggers‚ and utilized skills.
Many sites offer comprehensive DBT skills handouts alongside the diary cards‚ enhancing the user’s understanding and application of these techniques. Utilizing these free resources empowers individuals to actively participate in their therapeutic journey.
Websites Offering DBT Resources
Several websites specialize in providing DBT materials‚ including readily available Diary Card PDFs. Behavioral Tech is a prominent source‚ offering comprehensive DBT resources developed by Marsha M. Linehan and her associates.
Other valuable platforms include DBT Skills‚ which provides handouts and worksheets‚ and various mental health websites offering downloadable DBT tools. These sites often categorize resources by skill module – mindfulness‚ interpersonal effectiveness‚ emotional regulation‚ and distress tolerance.
Exploring these websites allows users to access a wealth of information and practical tools to support their DBT journey‚ all conveniently available as free PDF downloads.
Specific PDF Providers (e.g.‚ Behavioral Tech)
Behavioral Tech stands out as a leading provider of official DBT resources‚ including downloadable Diary Card PDFs. They offer materials directly linked to Marsha M. Linehan’s DBT Skills Training Manual‚ ensuring authenticity and alignment with core principles.
Additionally‚ websites compiling DBT handouts often host PDF versions of the Diary Card. These compilations frequently include variations tailored to different needs‚ offering options for tracking emotions‚ behaviors‚ and utilized skills.
Accessing these resources directly from Behavioral Tech or reputable compilation sites guarantees quality and supports effective DBT practice.
Using a DBT Diary Card Effectively
DBT Diary Cards maximize benefit with consistent daily completion and review alongside a therapist‚ revealing patterns and facilitating skill development for lasting change.
Daily Completion & Consistency
Consistent‚ daily completion of your DBT Diary Card is paramount for its effectiveness. Treat it as a non-negotiable appointment with yourself‚ dedicating even just 10-15 minutes each day.
Downloading a free DBT Diary Card PDF is a great start‚ but the real value lies in regular use. This practice builds self-awareness by tracking emotions‚ behaviors‚ and skills utilized.
Missed days diminish the ability to identify patterns and trends. Aim for accuracy‚ even when challenging‚ as honest self-reflection fuels progress in therapy and skill development‚ as outlined in Linehan’s manuals.
Reviewing Diary Cards with a Therapist
Regularly reviewing your completed DBT Diary Card with your therapist is a cornerstone of effective DBT treatment. Even utilizing a free DBT Diary Card PDF‚ the collaborative analysis unlocks deeper insights.
Your therapist can help identify patterns in emotions‚ behaviors‚ and triggers that you might miss independently. This process facilitates targeted skill application and addresses areas needing further development.
Discussing entries provides a safe space to explore challenging experiences and refine coping strategies‚ drawing upon Linehan’s DBT skills training. It’s a vital step in tracking progress and fostering self-awareness.
Identifying Patterns & Trends
Consistent use of a DBT Diary Card‚ even a free DBT Diary Card PDF download‚ allows for the identification of recurring emotional and behavioral patterns. Tracking data over time reveals triggers and vulnerabilities.
Noticing these trends is crucial for proactive intervention. Are certain situations consistently linked to intense emotions? Do specific behaviors escalate distress? Recognizing these connections empowers you to apply DBT skills preemptively.
This self-monitoring‚ guided by resources like Linehan’s DBT skills training materials‚ fosters greater self-awareness and facilitates more effective coping strategies.
Key DBT Skills Integrated with Diary Card Use
DBT Diary Cards‚ often accessed as a free PDF‚ directly support skill application‚ tracking mindfulness‚ emotional regulation‚ interpersonal effectiveness‚ and distress tolerance.
Utilizing these cards alongside DBT skills training enhances self-awareness and promotes consistent practice for lasting emotional wellbeing.
Mindfulness Skills & Diary Card Entries
DBT Diary Cards‚ frequently available as a free PDF download‚ provide a dedicated space to record mindful moments throughout the day. Entries can detail observations without judgment‚ a core tenet of mindfulness.
Specifically‚ the card allows tracking of “what” and “how” – detailing events and the corresponding emotional and physical sensations experienced. This practice‚ rooted in Marsha M. Linehan’s teachings‚ fosters present moment awareness.
Consistent recording helps identify patterns between triggers and reactions‚ strengthening the ability to observe emotions without being overwhelmed. Utilizing a DBT skills training manual alongside the card enhances understanding and application.
Ultimately‚ this integration cultivates a greater sense of self-awareness and emotional regulation.
Interpersonal Effectiveness & Recording Interactions
A free DBT Diary Card PDF offers a structured format to document interpersonal interactions‚ crucial for practicing Interpersonal Effectiveness skills. Users can record details of conversations‚ noting their own and others’ behaviors.
Entries should focus on applying DBT skills – assertiveness‚ building mastery‚ and maintaining self-respect – during interactions. This allows for objective review‚ identifying what worked well and areas for improvement.
Referencing DBT skills training handouts‚ often found alongside diary card resources‚ aids in accurately labeling skills used. Analyzing these records reveals patterns in communication styles and emotional responses.
Ultimately‚ this process fosters healthier relationships and improved communication skills.
Emotional Regulation & Tracking Emotional Shifts
Utilizing a free DBT Diary Card PDF is vital for tracking emotional experiences and practicing emotional regulation skills. The card provides space to record the intensity of emotions throughout the day‚ identifying triggers and subsequent shifts.
Individuals can document which DBT skills – like opposite action or distress tolerance – were employed to manage intense feelings. This allows for a clear understanding of skill effectiveness.
Consistent tracking‚ guided by resources from Marsha M. Linehan’s work‚ reveals patterns in emotional reactivity and helps pinpoint areas needing focused intervention.
This self-monitoring promotes increased emotional awareness and facilitates lasting change.
Distress Tolerance & Documenting Coping Mechanisms
A free DBT Diary Card PDF is instrumental in documenting the use of distress tolerance skills during challenging moments. Individuals can record the specific crisis situation and the intensity of their distress before intervention.
The card allows for detailed logging of coping mechanisms employed – such as self-soothing‚ distraction‚ or radical acceptance – and their perceived effectiveness.
Referencing DBT Skills Training Manuals‚ users can track which techniques provide the most relief and identify areas for skill refinement.
This process fosters self-reliance and builds a repertoire of healthy coping strategies.

Customizing Your DBT Diary Card
DBT Diary Card PDFs can be personalized! Adapt categories to track specific behaviors‚ create tailored trigger lists‚ and enhance self-monitoring for optimal results;
Modifying a free PDF ensures the card aligns with individual needs and therapeutic goals‚ maximizing its effectiveness.
Adapting the Card to Individual Needs
Utilizing a DBT Diary Card PDF doesn’t necessitate rigid adherence to a standard format. Individuals benefit greatly from tailoring the card to reflect their unique challenges and therapeutic objectives. Consider adding sections for specific problematic behaviors not initially included‚ or expanding the emotional intensity scale for greater nuance.
Personalization ensures the diary card becomes a truly effective self-monitoring tool. Downloadable free PDFs offer a convenient starting point‚ allowing for handwritten adjustments or digital modifications. This adaptability fosters a stronger connection to the process‚ promoting consistent daily completion and more insightful review sessions with a therapist. Remember‚ the goal is increased self-awareness!
Adding Specific Behavior Categories
When utilizing a DBT Diary Card PDF‚ proactively identify behaviors crucial to your recovery journey. Standard cards may not encompass all problematic actions. For example‚ if self-isolation is a key issue‚ create a dedicated category to track frequency and triggers. Similarly‚ impulsive spending or excessive social media use warrant specific tracking sections.
Downloading free PDFs provides a flexible base. Simply add rows or columns to accommodate these personalized categories. This focused tracking‚ informed by therapeutic goals‚ enhances self-observation. Detailed behavioral data‚ alongside emotional states‚ facilitates identifying patterns and applying appropriate DBT skills effectively.
Creating Personalized Trigger Lists
Leveraging a DBT Diary Card PDF‚ build a detailed list of personal triggers. These aren’t always obvious; they can be subtle situations‚ thoughts‚ or even times of day. A free PDF download offers space for customization. Note specific people‚ places‚ or internal experiences preceding emotional distress.
Categorize triggers (interpersonal‚ environmental‚ internal) for clarity. Regularly review and update this list alongside diary card entries. Identifying these precursors‚ using DBT skills‚ allows for proactive coping. This personalized approach‚ facilitated by the card‚ fosters self-awareness and reduces reactivity to challenging stimuli.

Beyond the PDF: Digital Diary Card Options
While DBT Diary Card PDFs offer accessibility‚ numerous apps and spreadsheet templates provide digital tracking alternatives for convenient‚ organized skill practice.
These digital formats often include features like data visualization and reminders‚ enhancing consistency and facilitating insightful pattern identification.
DBT Diary Card Apps
DBT Diary Card Apps represent a modern evolution beyond traditional DBT Diary Card PDFs‚ offering enhanced functionality and convenience for users actively engaged in therapy. These applications typically feature intuitive interfaces designed for daily tracking of emotions‚ behaviors‚ and utilized skills.
Many apps allow for customizable categories‚ personalized trigger lists‚ and the ability to record detailed descriptions of challenging situations. Furthermore‚ they often provide data visualization tools‚ enabling users to identify patterns and trends in their emotional experiences over time.
Digital formats also offer benefits like automated reminders‚ secure data storage‚ and easy sharing with therapists‚ fostering a collaborative approach to treatment and skill development. Several options are available on both iOS and Android platforms‚ catering to diverse user preferences.
Spreadsheet Templates for Tracking
Spreadsheet Templates offer a flexible alternative to DBT Diary Card PDFs‚ allowing for personalized tracking of emotions‚ behaviors‚ and skills within a familiar digital environment. Programs like Microsoft Excel or Google Sheets can be easily adapted to mimic the structure of a traditional diary card.
Users can customize columns to reflect individual needs‚ adding specific behavior categories or trigger lists. The formulas and charting features enable data analysis‚ revealing patterns and trends in emotional regulation and coping mechanisms.
These templates provide a cost-effective and accessible solution‚ particularly for individuals comfortable with spreadsheet software‚ offering a degree of control and customization not always found in pre-designed PDF formats or apps.

The Role of the Diary Card in DBT Treatment
DBT Diary Cards track therapeutic progress‚ facilitate skill development‚ and enhance self-awareness by documenting daily experiences and emotional shifts‚ even using free PDF versions.
Tracking Progress in Therapy
DBT Diary Cards serve as invaluable tools for monitoring a client’s journey throughout therapy‚ providing concrete data points for review with a therapist. Consistent use‚ even with readily available free PDF versions‚ allows for the identification of patterns in emotions‚ behaviors‚ and trigger situations.
This detailed tracking facilitates a more targeted approach to skill application‚ enabling therapists to assess the effectiveness of learned techniques. Observing trends over time‚ documented on the card‚ highlights areas of improvement and challenges‚ informing treatment adjustments. The diary card transforms subjective experiences into objective data‚ fostering collaborative progress monitoring.
Resources like Marsha M. Linehan’s manuals support this process‚ ensuring consistent application of DBT principles.
Facilitating Skill Development
Utilizing a DBT Diary Card‚ even a free PDF download‚ actively encourages the practice of newly learned skills in real-life situations. The card prompts individuals to record when and how they attempted to apply mindfulness‚ interpersonal effectiveness‚ emotional regulation‚ or distress tolerance techniques.
This documentation isn’t merely recording that a skill was used‚ but also assessing its effectiveness. Analyzing these entries‚ alongside a therapist‚ reveals which skills are most readily accessible and beneficial.
Resources from Linehan’s Skills Training Manual emphasize this iterative process‚ turning the diary card into a dynamic tool for skill refinement and mastery.
Improving Self-Awareness
Consistent use of a DBT Diary Card‚ accessible through free PDF downloads‚ dramatically enhances self-observation skills. By meticulously tracking emotions‚ behaviors‚ and triggering events‚ individuals begin to recognize patterns previously unnoticed.
This detailed record fosters a deeper understanding of personal reactions and vulnerabilities. The act of journaling itself promotes mindful attention to internal experiences‚ moving beyond reactive responses.
Linehan’s work highlights that increased self-awareness is foundational to DBT‚ and the diary card serves as a practical tool for cultivating this crucial element of therapeutic progress.
Understanding the Limitations of Diary Cards
DBT Diary Cards‚ even free PDF versions‚ rely on self-reporting‚ which can be subject to inaccuracies or unintentional biases in recollection.
Honest self-reflection is vital‚ but challenging‚ and cards aren’t a substitute for professional therapeutic guidance.
Potential for Inaccurate Reporting
DBT Diary Cards‚ including those accessed as free PDF downloads‚ depend heavily on the individual’s ability to accurately recall and record their experiences. Memory is fallible‚ and emotional states can distort perceptions‚ leading to incomplete or biased reporting.
Individuals might unintentionally minimize or exaggerate certain feelings or behaviors‚ impacting the card’s usefulness for identifying patterns. Furthermore‚ completing a diary card during moments of intense emotion can be particularly challenging‚ potentially resulting in less objective entries.
It’s crucial to acknowledge this inherent limitation and discuss any discrepancies with a therapist during review sessions.
The Importance of Honest Self-Reflection
Utilizing a DBT Diary Card‚ even a free PDF version‚ demands genuine self-reflection. The value isn’t simply in completing the card‚ but in truthfully documenting emotions‚ behaviors‚ and skill usage‚ regardless of perceived judgment.
Honest reporting‚ even when uncomfortable‚ allows for accurate pattern identification and facilitates more effective therapy. Avoiding self-deception is paramount; minimizing difficulties hinders progress.
This process fosters self-awareness and accountability‚ crucial components of DBT. A willingness to confront challenging truths‚ recorded on the diary card‚ unlocks the potential for meaningful change.

Resources for Further DBT Learning
Marsha M. Linehan’s foundational work and DBT Skills Training Manuals offer in-depth knowledge. Explore online courses and readily available free DBT Diary Card PDFs.
Marsha M. Linehan’s Work
Marsha M. Linehan is the pioneering developer of Dialectical Behavior Therapy (DBT)‚ and her contributions are foundational to the practice. Her DBT Skills Training Manual is a cornerstone resource‚ providing comprehensive tools for implementing skills training‚ including the vital Diary Card.
Linehan’s work emphasizes a balance between acceptance and change‚ and the Diary Card embodies this principle by facilitating self-observation and tracking of behaviors. Many resources offer free DBT Diary Card PDFs based on her original designs. These materials are invaluable for both therapists and individuals seeking to learn and apply DBT skills effectively‚ promoting emotional regulation and distress tolerance.
DBT Skills Training Manuals
DBT Skills Training Manuals‚ particularly those authored by Marsha M. Linehan‚ are essential resources for understanding and implementing Dialectical Behavior Therapy. These manuals contain reproducible handouts and worksheets‚ including the crucial DBT Diary Card‚ designed to track emotions and behaviors.
Many individuals seek free DBT Diary Card PDFs derived from these manuals to support their therapy journey. The manuals detail four core modules: mindfulness‚ interpersonal effectiveness‚ emotional regulation‚ and distress tolerance. Utilizing these resources‚ alongside consistent diary card completion‚ fosters self-awareness and facilitates skill development for managing challenging emotions.
Online DBT Courses & Workshops
Online DBT Courses & Workshops often incorporate the use of DBT Diary Cards as a core component of skills practice and self-monitoring. Participants frequently receive or are directed to resources for obtaining free DBT Diary Card PDFs to aid in daily tracking of emotions and behaviors.
These courses‚ building upon Marsha M. Linehan’s foundational work‚ emphasize the four key modules: mindfulness‚ interpersonal effectiveness‚ emotional regulation‚ and distress tolerance. Workshops provide guidance on effectively utilizing diary cards to identify patterns‚ apply learned skills‚ and ultimately‚ enhance emotional wellbeing and self-awareness.